Quick Summary
For most people with diabetes, well-fitted, low-pressure compression socks are generally safe and helpful for mild swelling and heavy legs—if you don’t have significant peripheral arterial disease (PAD) or other red-flag conditions, and you check your skin daily (especially if you have neuropathy). People with severe PAD/critical limb ischemia should not use compression unless a vascular specialist specifically prescribes it. Start low (mild pressure), fit carefully, and speak with a clinician if you have circulation problems, foot wounds, or loss of sensation.
Are compression socks safe if you have diabetes?

Usually yes—provided the pressure and fit are appropriate and contraindications are ruled out.
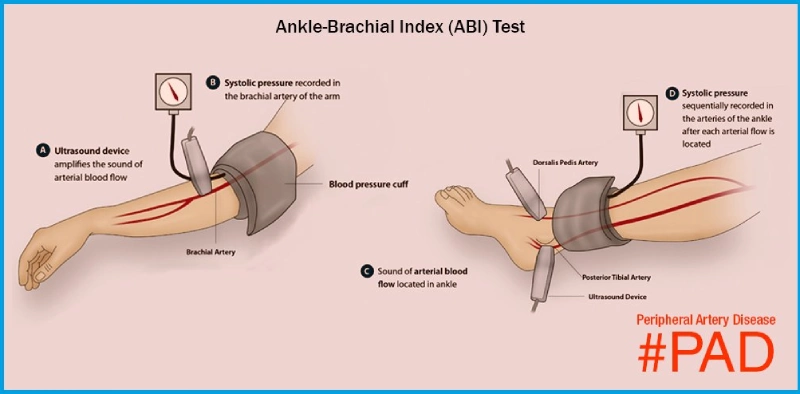
Extra caution is needed because neuropathy can blunt pressure/pain awareness (raising pressure-injury risk) and PAD can reduce blood flow. Clinicians therefore screen for PAD (often with an ankle–brachial index, ABI, and/or toe pressures) and check skin integrity before recommending compression.
Who should not wear compression socks (or must see a clinician first)?

Do not self-start compression; seek medical advice first if you have any of the following:
- Severe PAD / critical limb ischemia (very low ABI or toe pressures). This is a classic contraindication to compression unless a vascular specialist prescribes it.
- Active infection (cellulitis) or open wounds not yet under professional wound care.
- Marked foot deformity or very fragile skin (common in neuropathy) that makes pressure injury likely—requires individualized fitting and close monitoring.
- Uncertain circulation status (never screened for PAD, uncertain foot pulses) or rest pain in the feet. Get evaluated (often with ABI) before using compression.
Important: Diabetes is a major PAD risk factor. If you’ve never had vascular screening, or you have foot wounds, color changes, cool toes, or nighttime/rest pain, do not start compression without a clinician’s OK.
When are compression socks helpful for people with diabetes?

- Mild leg/ankle swelling from prolonged sitting/standing or travel, when circulation is adequate.
- Venous insufficiency/varicose veins coexisting with diabetes (after ruling out significant PAD).
- Post-edema control as part of a clinician-supervised plan.
Choosing a pressure level (how much “mmHg”?)
- Start low. For general leg fatigue or mild swelling, begin with mild compression (e.g., 15–20 mmHg; some may start at 8–15 mmHg). This is especially sensible while confirming you don’t have significant PAD and you’re building a habit of daily skin checks.
- Go higher only with guidance. 20–30 mmHg (or above) is typically reserved for specific diagnoses (e.g., chronic venous disease, edema) under clinical supervision, especially if you have diabetes, neuropathy, or arterial concerns. Higher pressure increases the risk of pressure injury if the fit is poor or sensation is reduced.
ABI quick guide (for context, not self-diagnosis):
≤ 0.90 suggests PAD; 0.41–0.90 indicates mild–moderate PAD; ≤ 0.40 indicates severe ischemia; > 1.30 may reflect vessel calcification and calls for alternative testing (e.g., toe pressures). Whether compression is appropriate—and at what pressure—depends on ABI/toe pressures and clinical judgment.
How to wear them safely (daily routine)

- On in the morning, off at night (unless your clinician advises otherwise).
- Daily foot checks: look for redness, indentations that don’t fade, blisters, drainage, color/temperature changes, or new pain—core diabetes foot-care advice.
- If you have reduced sensation (neuropathy), use a mirror or ask a family member to inspect.
- Proper donning: use gloves or a donning aid, smooth out wrinkles, and re-check the skin after 30–60 minutes on day one. Re-measure size if your weight or swelling pattern changes.
Risks to watch for (stop and call if you notice…)
- Increasing foot pain at rest, pale/cool toes, or new color changes (possible ischemia).
- Skin breakdown, blisters, or weeping areas under the sock or at the top band.
- New/worsening numbness or tingling after putting them on.
These are well-recognized warning signs in compression therapy and diabetic foot care.
FAQs
Are compression socks safe if I have diabetes?
Usually yes, with proper screening and fit. [See how compression helps], [how to size and fit]. Severe PAD remains a contraindication.
Which pressure should I pick first?
Begin with 8–15 mmHg or 15–20 mmHg if you don’t have PAD. Use 20–30 mmHg only with clinician guidance after circulation testing. [See pressure guide]
Who should avoid compression socks?
People with critical limb ischemia/severe PAD, active ulcers/infection, or severe neuropathy with unrecognized injuries should avoid self-starting compression and seek specialist care.
How do I put them on without hurting my skin?
Use gloves or a donning aid, smooth wrinkles, and check skin after 30–60 minutes the first day. Remove at night unless instructed.
What are the risks for people with diabetes?
The big ones are ischemia in hidden PAD and pressure injury in neuropathy. That’s why ABI/toe pressure testing and daily checks matter.
