Introduction: Understanding Compression Socks and Their Rising Popularity
Brief Overview of Compression Socks
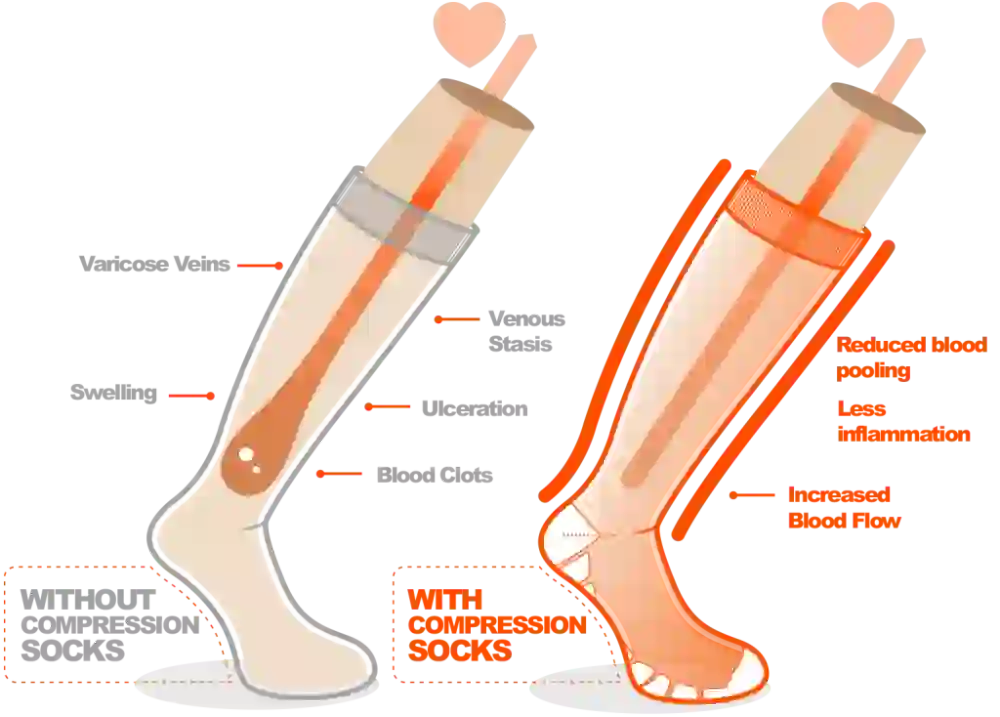
Compression socks are specially knit garments that apply graduated pressure to the legs, strongest at the ankle and gradually decreasing toward the knee or thigh. Unlike regular socks, they’re engineered to support venous return—helping blood flow upward against gravity. Originally developed for medical use, modern compression wear comes in a variety of styles and pressures suited to both clinical settings and everyday life.

Growing Popularity Among Different Demographics
Once confined to hospitals and long-haul flights, compression socks now appear in gyms, offices, and grocery aisles. Travelers use them to ward off leg swelling on long flights. Office workers and teachers wear them to combat fatigue during standing or sitting marathons. Athletes adopt compression for performance and recovery. Even pregnant women and older adults rely on these socks to ease discomfort. This broad appeal reflects both growing awareness of circulatory health and improvements in design, color, and comfort.
Preview of Health Benefits and Concerns
Compression therapy promises many benefits: reduced swelling, lower risk of blood clots, relief from varicose vein pain, and enhanced leg comfort. Yet it’s not risk-free. Ill-fitting or overly tight socks can impede circulation, and certain medical conditions contraindicate their use. In this guide, we’ll dissect how compression works, review evidence for cardiovascular and vein health, explore daily comfort uses, and highlight safety considerations so you can decide whether compression socks are right for you.
The Science Behind Compression Therapy: How Do Compression Socks Work?
Explanation of Graduated Compression
Graduated compression means pressure is highest at the ankle—often around 20–30 mmHg—and decreases progressively up the leg. This gradient mimics the action of healthy veins and calf muscles, which naturally pump blood back to the heart. By externally supporting this mechanism, compression socks amplify venous return, reducing the volume of blood pooled in the lower legs.
Blood Flow Mechanics and Venous Return
Inside each leg, tiny one-way valves prevent backflow as blood moves upward. When these valves weaken—due to age, pregnancy, or prolonged immobility—blood can pool, causing swelling and discomfort. The firm ankle pressure of compression socks narrows the vein diameter slightly, increasing flow velocity. As you walk, the calf muscles further squeeze veins against the sock’s support, propelling blood upward more efficiently.
Scientific Principles Behind Compression Therapy
Compression therapy rests on Poiseuille’s law and the concept of shear stress: reducing vessel diameter increases flow rate, while external pressure reduces hydrostatic pressure within veins. Clinical studies demonstrate that appropriate compression can decrease capillary filtration, minimize edema, and improve lymphatic drainage. Together, these effects translate into measurable reductions in leg circumference and subjective improvements in heaviness and ache.
Cardiovascular Benefits: Preventing Blood Clots and Deep Vein Thrombosis
Risk Factors for DVT
Deep vein thrombosis (DVT) occurs when a clot forms in a deep vein, typically in the calf or thigh. Risk factors include prolonged immobility (long flights or bed rest), recent surgery, cancer, obesity, smoking, and genetic clotting disorders. Symptoms may be subtle—leg swelling, warmth, or a dull ache—and left untreated, DVT can lead to life-threatening pulmonary embolism.
How Compression Socks Help Prevent Clotting
By enhancing venous return, compression socks reduce the stasis of blood that predisposes to clot formation. The graduated pressure raises flow velocity, lowering the risk that platelets will adhere to vessel walls and initiate clotting. In high-risk settings—post-surgical recovery or long-distance travel—wearing 15–30 mmHg stockings has become standard preventive care.
Research Evidence on Effectiveness
Multiple randomized controlled trials and meta-analyses confirm that compression reduces DVT incidence in hospitalized patients and travelers alike. One landmark study showed a 60% reduction in post-surgical DVT when patients wore thigh-high 20–30 mmHg compression socks versus no socks. Other research highlights fewer leg symptoms and lower markers of coagulation activation among compression users, reinforcing their role in clot prophylaxis.
Addressing Varicose Veins: Can Compression Socks Help?
Causes of Varicose Veins
Varicose veins arise when vein walls weaken and valves fail, allowing blood to pool and vessels to dilate. Contributing factors include genetics, prolonged standing or sitting, obesity, pregnancy, and age. These bulging, twisted veins can cause aching, heaviness, and cosmetic concerns. Left untreated, varicose veins may lead to skin changes or ulcers.
Compression Therapy as a Management Strategy
Graduated compression socks—typically in the 20–30 mmHg range—apply steady pressure to support vein walls and encourage blood flow back toward the heart. This external support reduces venous pressure, lessening vein distension and associated symptoms. Unlike invasive procedures, compression therapy is non-invasive, low-cost, and free of medication side effects. Worn daily, it can help manage mild to moderate varicosities and slow progression.
Expectations vs. Reality for Varicose Vein Treatment
Compression socks won’t eliminate varicose veins but can offer symptom relief and cosmetic improvement over time. Patients often report reduced leg aching, decreased swelling, and a lighter sensation after several weeks of consistent wear. For persistent or severe cases, doctors may recommend combining compression with treatments such as sclerotherapy or endovenous laser therapy. In those scenarios, compression socks support healing and maintain results post-procedure.
Relief for Tired and Sore Legs: Compression Socks for Daily Comfort
Causes of Leg Fatigue and Soreness
Leg fatigue stems from fluid accumulation, muscle overuse, and reduced venous return. Long periods of standing—in retail, hospitality, or on factory floors—exert constant downward pressure, while prolonged sitting—during commutes or desk work—slows circulation. Both scenarios lead to pooling of blood and interstitial fluid in the calves and ankles, generating heaviness, cramps, and discomfort.
How Compression Improves Comfort
By providing graduated pressure (highest at the ankle, tapering upward), compression socks enhance venous return and lymphatic drainage. Improved flow reduces fluid buildup and metabolite accumulation, which translates into less swelling and cramping. Additionally, gentle support around the calf muscles decreases muscle oscillation during movement, cutting down on post-activity soreness. Many users find that wearing 15–20 mmHg socks during work hours yields noticeably lighter, more energized legs by day’s end.
Ideal Compression Levels for Daily Wear
For general comfort and prevention of everyday leg fatigue, light to moderate compression (15–20 mmHg or 20–30 mmHg) is recommended. Lighter grades suit those with minimal swelling or who stand intermittently. Moderate grades better address noticeable puffiness or mild vein issues. Choose knee-high styles for ease of use; thigh-high or pantyhose styles are options if you require additional support or have pronounced thigh-level pooling.
Athletic Performance and Recovery: Compression Socks for Active Individuals
Benefits During Exercise
Compression socks can enhance proprioception and reduce muscle vibration during runs, jumps, and rapid direction changes. Improved stability may decrease injury risk, while the external support lessens perceived effort. Research indicates that moderate compression (20–30 mmHg) can marginally improve endurance performance by optimizing blood flow and reducing early muscle fatigue.
Post-Workout Recovery Advantages
After intense training or competition, muscles often experience micro-tears and inflammation. Wearing compression socks post-exercise aids in efficient removal of metabolic byproducts like lactate. Graduated pressure promotes faster venous return and reduces swelling, potentially shortening recovery time. Athletes frequently report reduced soreness and improved readiness for subsequent sessions when they include compression in their recovery routine.
Types of Compression Gear for Different Activities
For running and court sports, knee-high socks or calf sleeves in 15–20 mmHg or 20–30 mmHg offer balanced support and freedom of movement. Cyclists and rowers may prefer full-leg or thigh-high tights. High-intensity interval training and weightlifting athletes often choose tighter, 20–30 mmHg calf sleeves for focused support. Always match compression level and garment length to the demands of the sport and personal comfort preferences.
Medical Applications: When Doctors Recommend Compression Therapy
Common Medical Conditions Requiring Compression
Physicians often prescribe compression socks for conditions like chronic venous insufficiency, lymphedema, and post-thrombotic syndrome. In chronic venous insufficiency, weakened vein valves allow blood to pool, causing swelling and discomfort; graduated compression counteracts these effects. Lymphedema patients benefit from firm, consistent pressure to encourage lymphatic fluid drainage. After a DVT, post-thrombotic syndrome can develop—persistent leg pain, swelling, and skin changes—which compression therapy helps manage.
Prescription vs. Over-the-Counter Options
Over-the-counter (OTC) compression socks typically come in 15–20 mmHg and 20–30 mmHg grades and are suitable for mild symptoms and preventive use. For more severe conditions or precise treatment, doctors may prescribe custom-fit garments up to 30–40 mmHg, often requiring specialist measurement. Prescription socks ensure exact graduated pressure profiles tailored to individual venous anatomy and medical needs. Insurance may cover these higher-grade, custom-fitted options when medically justified.
Working with Healthcare Providers
Always consult a healthcare professional before starting compression therapy for medical issues. Your provider will evaluate your vascular health, measure your legs correctly, and recommend the appropriate mmHg level and sock length. Periodic follow-ups allow your doctor to adjust compression strength as your condition improves or changes. Close collaboration ensures safety and maximizes therapeutic benefit while minimizing potential complications.
Choosing the Right Compression Level: Understanding mmHg Ratings
Explanation of mmHg Measurement
The term mmHg (“millimeters of mercury”) refers to the pressure exerted by the sock, measured in the same units as blood pressure. A sock rated 20–30 mmHg applies that amount of downward pressure at the ankle, gradually easing up the calf. This gradient pressure design supports natural venous return mechanisms and helps prevent fluid accumulation.
Different Compression Levels and Their Purposes
- Light (8–15 mmHg): Ideal for mild leg fatigue, minor swelling during travel, and preventive wear.
- Moderate (15–20 mmHg): Suited for daily comfort, mild varicose veins, and routine DVT prevention.
- Firm (20–30 mmHg): Prescribed for moderate varicosities, post-thrombotic syndrome, and more pronounced edema.
- Extra-Firm (30–40 mmHg): Reserved for severe venous disease, lymphedema management, and post-surgical support—use only under medical supervision.
Guidelines for Selecting Appropriate Compression
Assess your symptoms first: mild discomfort and occasional swelling call for light to moderate grades. If you have diagnosed vein disease or significant edema, discuss firm or extra-firm options with your doctor. Consider activity level: those on their feet most of the day may need higher compression for lasting relief. Always verify fit and comfort; too-tight socks can harm more than help.
Potential Risks and Side Effects: When Compression Socks Might Not Be Good for You
Contraindications for Compression Wear
Compression therapy is not safe for everyone. People with peripheral arterial disease (PAD) risk further restricting blood flow if they wear compression socks. Severe congestive heart failure patients should also avoid unmonitored compression, as moving pooled fluid back to the heart may overburden cardiac function. Always have vascular health assessed before beginning compression therapy.
Common Side Effects and Discomfort
Improper fit or excessive compression can cause numbness, tingling, or skin indentations. Socks that roll down or bunch can create tourniquet-like pressure points. Allergic reactions to dyes or elastic fibers may lead to itching or dermatitis. If any of these issues arise, discontinue use and re-evaluate fit, material, and compression strength.
When to Discontinue Use
Stop wearing compression socks immediately if you experience increased pain, color changes in your toes or feet, swelling above the sock’s edge, or signs of skin breakdown. Seek medical advice if discomfort persists despite correct sizing. A personalized assessment will help determine whether a lower compression level or alternative therapy is more appropriate.
Proper Fit and Sizing: Ensuring Maximum Benefit and Comfort
Importance of Correct Sizing
An optimal fit is crucial for compression efficacy. Socks that are too tight can constrict circulation, while loose socks fail to provide the graduated pressure needed. Properly sized compression garments deliver consistent force where it’s needed most—helping blood travel upward and reducing fluid buildup. Investing time in accurate measurement prevents discomfort, skin indentations, and wasted expense on returns or replacements.
Measuring Techniques
Begin by measuring your ankle circumference at the narrowest point just above the ankle bone. Next, measure the widest part of the calf. If you’re choosing thigh-high or full-leg styles, record the thigh circumference at its largest section and measure leg length from heel to under the knee or top of the thigh. Always measure first thing in the morning before swelling develops. Record each measurement in centimeters, and compare against the manufacturer’s sizing chart. If you fall between two sizes, select the larger to avoid excessive tightness.
Signs of Improper Fit
Even with correct measurements, fit can vary by brand. Watch for these red flags:
- Excessive tightness: Numbness, tingling, or pain in the foot or calf.
- Slippage or sagging: Socks rolling down or bunching behind the knee, indicating an overly large size or weak elastic.
- Uneven pressure: Wrinkles or pinches around the ankle or calf suggest the sock isn’t distributing pressure properly.
If you notice any of these signs, re-measure or try a different size or style to achieve the intended therapeutic effect.
Daily Wear Guidelines: How Long Should You Wear Compression Socks?
Recommended Duration for Different Needs
- Preventive use: For travel or long periods of standing, wear compression socks for the duration of the activity—often 4–8 hours.
- Therapeutic use: When managing vein disease or post-surgical recovery, daily wear of 8–12 hours is common, as advised by your healthcare provider.
- Athletic use: Athletes may wear compression during workouts and for 1–2 hours post-exercise to aid recovery.
Putting On and Taking Off Techniques
Always put socks on before swelling sets in—ideally first thing in the morning. Turn the sock inside out to the heel, insert your foot, align the toe seam, then gently pull the rest up your leg, smoothing out wrinkles. To remove, peel the sock down slowly, avoiding sharp bends that can damage fibers. Special donning aids or gloves can help those with limited hand strength.
Nighttime Wear Considerations
Most compression socks are designed for daytime use. Unless prescribed for specific medical conditions, avoid wearing them while sleeping to let skin breathe and prevent excessive overnight pressure. If your doctor recommends overnight wear—for severe edema or lymphedema—use a lower compression grade (8–15 mmHg) and reapply in the morning.
Care and Maintenance: Extending the Life of Your Compression Garments
Washing and Drying Best Practices
Machine-wash compression socks on a gentle cycle using cold water and a mild, pH-neutral detergent. Skip bleach and fabric softeners—they degrade elastic fibers and diminish compression over time. After washing, reshape each sock and lay flat to air dry. Avoid tumble drying and direct sunlight, which can weaken fibers and cause fading.
Signs of Wear and Replacement Timing
Compression efficacy diminishes as elastic fibers break down. Replace your socks when you notice:
- Reduced snugness around the ankle and calf.
- Visible thinning in high-wear areas like the heel and toe.
- Loss of elasticity or sock sagging after wear.
Generally, replace compressive hosiery every 3–6 months, or sooner if you wear them daily.
Storage Recommendations
Store your compression socks flat or rolled loosely—avoid hanging by the cuff, which stretches the top band. Keep them in a cool, dry place away from direct heat or moisture. For travel, pack socks in a protective pouch to prevent snagging on zippers or rough materials. Proper storage preserves elasticity and ensures consistent performance.
Conclusion: Making an Informed Decision About Compression Therapy
Compression socks offer a versatile, non-invasive approach to managing a range of leg and circulatory issues—from preventing deep vein thrombosis to easing varicose vein discomfort and daily leg fatigue. Their effectiveness hinges on selecting the right mmHg level, ensuring precise fit through accurate measurements, and adhering to proper wear guidelines. Light to moderate grades (15–30 mmHg) suit most preventive and comfort needs, while higher grades (30–40 mmHg) require medical supervision.

Scientific principles—graduated pressure that promotes venous return, reduces capillary filtration, and enhances lymphatic drainage—underlie the proven cardiovascular and vein-health benefits of compression therapy. Athletes gain performance and recovery advantages, travelers and desk-bound workers avoid swelling and clot risk, and patients with chronic venous insufficiency or lymphedema achieve symptom relief. Yet compression is not without potential risks: contraindications like peripheral arterial disease or poorly fitted garments can worsen circulation or cause skin issues.
A personalized approach—consulting healthcare providers for medical indications, using manufacturer sizing charts for proper fit, and choosing fabrics and designs that match individual lifestyles—ensures you reap the full rewards. Routine care and timely replacement preserve compression efficacy over months of use. By weighing benefits, understanding limitations, and following best practices, you can decide with confidence whether compression socks belong in your daily regimen or clinical protocol.
FAQ
Are compression socks safe to wear every day?
Yes—light to moderate grades (15–30 mmHg) are generally safe for daily preventive or comfort use; higher grades need medical guidance.
Can compression socks help with plantar fasciitis or foot pain?
They can relieve some foot discomfort by improving circulation and providing arch support, but they’re not a primary treatment for plantar fasciitis.
Should I wear compression socks while sleeping?
Nighttime wear isn’t recommended unless prescribed for specific conditions; most wear guidelines advise removal before bed.
How tight should compression socks feel?
They should be snug without causing numbness, tingling, or pain—firm at the ankle and gradually less tight up the calf.
Can compression socks cause skin problems?
Rarely—improper fit, material allergies, or prolonged wear without breaks can lead to irritation, indentations, or dermatitis.
