Introduction: Understanding the Connection Between Diabetes and Foot Health
Diabetes creates unique challenges for foot health that extend far beyond simple comfort considerations, making specialized footwear solutions like diabetic socks essential components of comprehensive care rather than optional accessories. The combination of peripheral neuropathy affecting sensation, potential circulatory impairment reducing healing capacity, and elevated infection risk creates a perfect storm of foot vulnerability for many diabetic individuals. This comprehensive guide explores the specific ways diabetic socks address these challenges, the essential features that distinguish quality options from ineffective alternatives, and how to integrate these specialized garments into broader foot care strategies for optimal health outcomes. By understanding both the science behind diabetic sock design and the practical considerations for daily use, readers can make informed decisions that potentially prevent serious complications while enhancing everyday comfort. This knowledge proves particularly valuable given the significant variation in product quality across the expanding diabetic sock marketplace, where marketing claims don’t always align with therapeutic benefits for this medically vulnerable population.

Understanding Peripheral Neuropathy
The Neurological Impact of Diabetes
Peripheral neuropathy, a common diabetes complication, affects up to half of long-term diabetic patients. It damages nerves, often starting in the feet, causing symptoms from increased sensitivity to complete numbness. High blood sugar, oxidative stress, and inflammation damage nerve fibers and protective sheaths. This leads to abnormal sensations like burning or tingling, sometimes without pain to warn of injuries. Without these warnings, minor foot injuries can go unnoticed and worsen, making preventive care essential. Diabetic socks play a vital role in protecting vulnerable feet, going beyond comfort to help prevent serious complications.
How Neuropathy Increases Foot Risk
Neuropathy causes sensory loss that allows injuries to worsen unnoticed. Autonomic nerve damage alters sweating, causing either dry, cracked skin or excessive moisture, both raising infection risks. Motor neuropathy changes foot structure, creating pressure points from deformities like hammertoes or collapsed arches. These changes increase calluses and risk of wounds. Diabetic socks address these issues with features like moisture control, pressure cushioning, and seamless designs. These targeted solutions help protect diabetic feet by managing the specific risks caused by neuropathy rather than offering basic comfort alone.
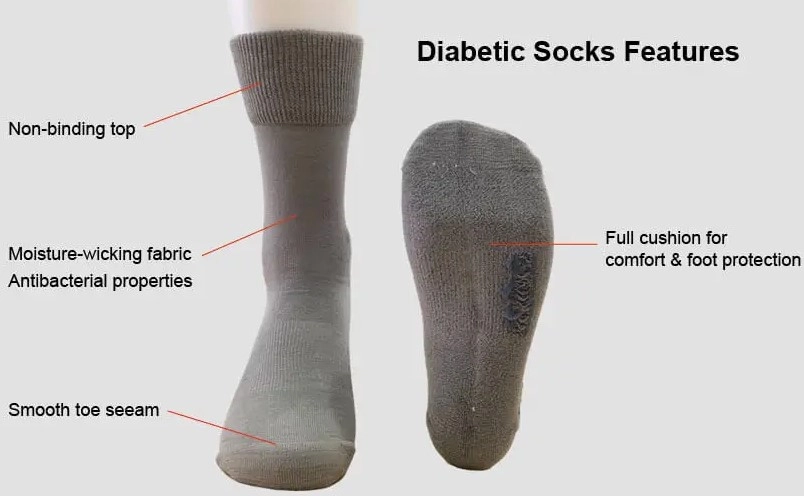
Essential Features of Diabetic Socks
Non-Restrictive Design
Diabetic socks use non-binding tops to avoid cutting off circulation, crucial for sensitive diabetic feet. They offer a gentle, graduated fit without tight compression, preventing pressure points that can reduce blood flow. The toe box is wider and deeper to accommodate natural foot shape and deformities like hammertoes. Stretch panels at flex points like ankles and insteps allow movement without tightness or rubbing. These features ensure the socks stay in place without compromising circulation, a key need for diabetic vascular health.
Moisture Management
Moisture control is vital to prevent infections common in diabetic feet. Diabetic socks use moisture-wicking fibers that move sweat away from the skin to the outer layers for evaporation, maintaining balanced hydration. Some include ventilation zones in high-sweat areas for extra breathability. Antimicrobial treatments inhibit bacteria and fungi, reducing odor and infection risk. This is especially important as neuropathy can prevent wearers from sensing moisture buildup, which otherwise leads to skin problems.
Protective Cushioning
Targeted cushioning protects high-pressure areas like heels, balls of feet, and toe tips to prevent ulcers. Unlike regular socks, diabetic socks focus padding where weight and pressure concentrate, redistributing force and reducing injury risk. They use durable materials that keep thickness under pressure and may include gel or silicone inserts for added protection. This helps compensate for lost sensation in neuropathic feet, offering critical protection beyond comfort.
Selecting the Right Diabetic Socks
Material Considerations for Different Needs
The specific materials used in diabetic socks significantly impact both their therapeutic effectiveness and subjective comfort, with optimal choices varying based on individual needs and conditions. Natural fibers like cotton provide excellent softness and breathability but retain moisture when wet—potentially problematic for those with heavy perspiration or active lifestyles. Bamboo offers natural antimicrobial properties with superior moisture management compared to cotton, making it valuable for infection-prone individuals, though often at higher price points. Wool blends provide excellent temperature regulation for those with circulatory impairment causing cold feet, with modern merino options offering softness without the itchiness associated with traditional wool. Synthetic performance fibers like polyester and nylon engineered specifically for moisture management offer superior wicking capabilities and durability, though some individuals find them less comfortable against sensitive skin compared to natural alternatives. For those with specific sensitivities, copper or silver-infused options provide enhanced antimicrobial protection through metallic ions that inhibit bacterial and fungal growth, potentially reducing infection risk beyond what standard materials offer. The ideal material choice depends on individual priorities—whether maximum moisture control, temperature regulation, antimicrobial protection, or sensory comfort—making material selection a personalized decision rather than a one-size-fits-all recommendation for the diverse needs within the diabetic population.
Choosing the Right Thickness and Length
Selecting appropriate thickness and length for diabetic socks requires balancing multiple factors including shoe fit, seasonal conditions, and specific foot protection needs. Thickness directly impacts both protective cushioning and shoe fit, with thicker options providing enhanced pressure distribution but potentially creating fit issues in shoes sized for thinner hosiery. Many individuals benefit from having multiple thickness options available—thinner socks for dress shoes or warm weather and thicker versions for athletic shoes or cold conditions—rather than attempting to find a single solution for all situations. Length selection involves both practical and medical considerations, with crew or knee-high styles providing extended protection for those with circulation concerns affecting the entire lower leg, while ankle-height options offer easier application and better heat management during warm weather. Some individuals with significant edema or venous insufficiency alongside diabetes benefit from specialized diabetic compression socks that combine non-restrictive tops with graduated mild compression—providing circulatory support without the potential constriction risks of standard compression hosiery. These thickness and length considerations highlight why many diabetic individuals maintain wardrobes of specialized socks for different activities and conditions rather than seeking single solutions, acknowledging that optimal protection requires adapting sock choices to specific situations rather than compromising with one-size-fits-all approaches that might create new risks while addressing others.
Integrating Diabetic Socks into Daily Foot Care
Establishing an Effective Sock Rotation
Maintaining an adequate supply of diabetic socks enables consistent protection through proper rotation practices that extend beyond simple cleanliness considerations. Most foot care specialists recommend owning at least 7-10 pairs of diabetic socks, allowing fresh application daily with buffer for laundry cycles. This quantity ensures clean socks for each wearing—crucial for infection prevention—while avoiding the temptation to reuse socks that might harbor moisture or contaminants. Beyond quantity, effective rotation involves varying sock types based on daily activities, with more heavily cushioned options for high-activity days and lighter versions for sedentary periods. Seasonal rotation proves equally important, with thinner moisture-focused options during warm months and thermal-regulating versions for colder periods when circulation challenges often intensify. Some individuals benefit from morning/evening rotation, changing socks midday to address accumulated moisture and provide fresh cushioning when feet typically swell during later hours. This comprehensive rotation approach acknowledges that even the most advanced diabetic socks provide optimal protection only when maintained in clean, dry condition and matched appropriately to specific daily needs rather than worn beyond their effective period or in situations mismatched to their design parameters. While representing additional investment compared to conventional hosiery, this robust sock supply ultimately proves cost-effective by reducing complication risks that might otherwise lead to significant medical interventions and associated expenses.
Daily Inspection and Replacement Protocols
Regular inspection and timely replacement of diabetic socks represent crucial components of effective foot care routines, particularly for those with sensation loss who cannot rely on discomfort to signal when socks no longer provide adequate protection. Daily visual inspection should check for thinning cushioning, elastic deterioration, holes or weak spots developing at pressure points, and any hardened areas that might create new pressure against vulnerable skin. Beyond visible damage, compression testing between fingers can identify cushioning that has compacted beyond its protective capacity despite maintaining normal appearance. Most quality diabetic socks maintain effective protection for approximately 4-6 months of regular wear and washing before requiring replacement, though this varies based on activity level, washing methods, and individual gait patterns that create different wear patterns. Some manufacturers incorporate “replacement indicators” like colored threads that become visible when cushioning compresses beyond effective levels or binding that loosens to signal elasticity loss. These objective indicators prove particularly valuable for those with neuropathy who cannot feel the reduced protection that occurs gradually over time. Establishing calendar-based replacement schedules—typically every 3-6 months depending on usage patterns—provides additional protection by ensuring regular rotation of fresh socks into use before protection deteriorates, acknowledging that prevention through proactive replacement costs significantly less than treating complications that might develop from continued use of inadequately protective worn-out diabetic socks.
Combining Socks with Comprehensive Foot Care
Daily Foot Inspection Routine
Diabetic socks provide optimal protection only when integrated into comprehensive foot care routines centered around thorough daily inspection practices. This inspection should occur at consistent times—typically evening when removing socks and morning before application—creating bookend examinations that catch any developing issues before they progress. The inspection process should follow systematic patterns covering all foot surfaces, including often-overlooked areas between toes and the posterior heel where visual examination requires additional effort. Beyond visual inspection, gentle tactile assessment helps identify temperature changes, swelling, or textural differences that might indicate developing problems before visible signs appear. Digital photography proves valuable for those with flexibility limitations, using phone cameras to capture images of foot undersurfaces for visual inspection when direct viewing proves challenging. Temperature assessment using the back of the hand can identify subtle inflammation suggesting potential infection or pressure injury developing beneath the skin surface before external signs appear. This inspection routine should occur regardless of symptom presence, acknowledging that neuropathy often masks warning signs until damage progresses significantly. When concerns arise during inspection, prompt professional evaluation should follow rather than waiting for symptoms to intensify or self-treating potential complications. This proactive inspection approach recognizes that diabetic socks represent one component of protection rather than complete solutions, with their effectiveness dependent on catching and addressing problems early before they progress to stages requiring advanced interventions beyond what specialized hosiery can address.
Proper Sock Application Techniques
The manner in which diabetic socks are applied significantly impacts their protective benefits, with proper techniques ensuring optimal positioning without creating new risks during the application process. Before application, visual inspection of the sock interior should check for foreign objects, seam irregularities, or fabric bunching that might create pressure points once applied. The recommended application approach involves gathering the sock from top to toe, creating a compact cylinder that can be placed over the toes and then gradually unrolled up the foot and leg without dragging fabric across vulnerable skin. This rolling technique distributes the fabric evenly while minimizing the shearing forces that might damage fragile skin during application. For those with limited dexterity or flexibility, various assistive devices facilitate independent application without requiring excessive bending or pulling that might create injury risks or balance challenges during the process. Proper positioning verification after application ensures therapeutic benefits, with key checkpoints including smooth fabric distribution without wrinkles, proper alignment of cushioned areas with corresponding foot structures, and appropriate height without rolling or bunching that might create pressure bands. These application considerations help maximize the protective benefits diabetic socks provide while minimizing risks that improper application might create—acknowledging that even the most advanced diabetic socks deliver optimal protection only when properly positioned on the foot without application-induced complications that might counteract their protective design features.
Advanced Options for Specific Needs
Copper and Silver-Infused Diabetic Socks
For individuals with recurrent fungal infections or persistent foot odor alongside diabetes, metal-infused diabetic socks offer enhanced antimicrobial protection beyond standard options. These specialized socks incorporate copper or silver particles bonded directly to fabric fibers, creating permanent antimicrobial properties that remain effective throughout the garment’s useful life rather than washing out like topical treatments. The antimicrobial mechanism involves metal ions gradually releasing onto skin surfaces, disrupting microbial cell membranes and metabolic processes to inhibit growth of bacteria and fungi responsible for both odor and infection. Research indicates these metal-infused fabrics can reduce microbial counts by 99.9% compared to untreated materials, potentially creating significantly more hygienic environments for vulnerable diabetic feet. Beyond infection prevention, some users report reduced inflammation and improved wound healing when using copper-infused options, though clinical evidence supporting these additional benefits remains preliminary. The primary disadvantages involve higher cost compared to standard diabetic socks and occasional skin sensitivity in individuals with metal allergies. These specialized options prove particularly valuable for those with histories of recurrent athlete’s foot, persistent interdigital infections, or problematic foot odor despite good hygiene practices—situations where the enhanced antimicrobial protection justifies the additional investment compared to standard diabetic socks that might not adequately address these specific challenges alongside their basic protective functions.
Thermal-Regulating Options for Circulatory Challenges
Individuals managing both diabetes and circulatory impairment often experience temperature regulation challenges that standard diabetic socks inadequately address, creating needs for specialized thermal-regulating options. These advanced socks utilize various technologies to maintain optimal foot temperature despite compromised circulation, with some incorporating phase-change materials that absorb excess heat when feet become warm and release stored heat when temperatures drop—creating more stable microenvironments than conventional insulation. Other designs utilize hollow-core fibers that trap warm air near skin surfaces without creating excessive insulation that might promote unwanted perspiration during activity transitions. Far-infrared options incorporate ceramic particles that reflect the body’s natural heat back toward the skin, potentially increasing local circulation through gentle warming without external heat sources that might create burn risks for those with sensation loss. These thermal-regulating features prove particularly valuable during seasonal transitions when temperature fluctuations challenge circulatory adaptation, or for those experiencing significant temperature differences between feet indicating vascular compromise requiring special attention. While typically more expensive than standard diabetic socks, these specialized thermal options often reduce dependency on external warming methods like heating pads that create burn risks for neuropathic feet, potentially offering both safety and comfort advantages that justify their premium pricing for those managing the combined challenges of diabetes and circulatory impairment affecting temperature perception and regulation in the extremities.
Conclusion: A Critical Component of Diabetic Foot Care
Diabetic socks represent far more than simple accessories or comfort items—they function as critical protective tools in the comprehensive management of diabetes-related foot health challenges. By addressing the specific vulnerabilities created by peripheral neuropathy through specialized design features, these purpose-built garments help bridge the protection gap created when sensation loss removes natural warning systems that would otherwise alert individuals to developing problems. The thoughtful selection and proper use of appropriate diabetic socks can significantly reduce complication risks while enhancing everyday comfort for those navigating the complex intersection of diabetes and foot health.

As diabetes care continues evolving, diabetic sock technology advances alongside it, with increasingly specialized options addressing specific needs within this diverse population. By understanding both the essential features that define quality diabetic socks and how to integrate them into comprehensive foot care routines, individuals can make informed choices that support long-term foot health despite the challenges diabetes presents. If you’re looking to customize diabetic socks tailored to your product goals or patient needs, visit our website to explore professional solutions designed by Max Hosiery—a trusted manufacturer in delivering comfort, safety, and performance in every pair.
FAQ Section
How are diabetic socks different from regular socks?
Diabetic socks have non-binding tops to avoid restricting circulation, seamless designs to prevent pressure points, moisture-wicking fabrics to reduce infection risk, and extra cushioning for sensitive areas. These features address diabetes-related foot problems that regular socks don’t.
How many pairs of diabetic socks should I own?
Experts suggest 7-10 pairs to ensure fresh socks daily and allow laundry rotation. Multiple pairs also help adapt to activity levels and seasons, with cushioned socks for active days and lighter ones for rest or warm weather.
Can I wear diabetic socks overnight?
Generally, it’s best to remove socks during sleep for skin breathing and foot checks. Exceptions apply if a doctor advises overnight use for severe circulation issues with proper monitoring.
How often should diabetic socks be replaced?
Replace diabetic socks every 4-6 months as cushioning and elasticity wear out. Usage and washing affect timing. Some brands include wear indicators to signal replacement time.
Are compression socks safe for diabetic patients?
Standard compression socks may pose risks for diabetics. However, specially designed diabetic compression socks with mild pressure and non-binding tops can be safe and helpful when prescribed by a healthcare professional.
