Introduction
What Is mmHg in Compression?
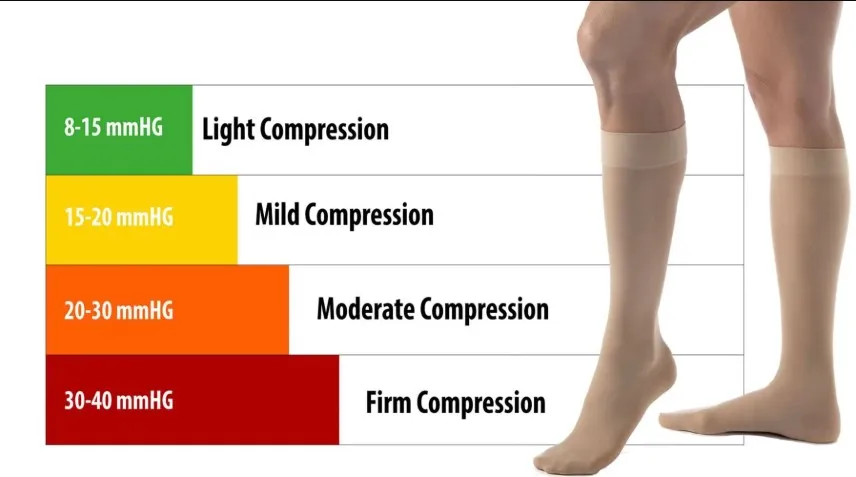
The term “mmHg” stands for millimeters of mercury, a unit of pressure originally used in blood pressure measurement. In compression garments, the mmHg value indicates how much squeezing force the fabric applies to your limbs. A sock labeled 20–30 mmHg applies firm, graduated pressure—highest at the ankle and tapering upward—to support circulation. Understanding this scale helps you choose the level of compression that matches your needs, whether you’re easing mild swelling or managing more pronounced vein issues.
Why mmHg Matters for Pregnant Women
During pregnancy, your blood volume increases dramatically, and growing uterine weight can slow blood flow in the lower limbs. The right mmHg grade helps counteract this by gently pushing fluid and blood back toward your heart, reducing ankle puffiness and leg fatigue. If you select too low a pressure, you may see little benefit; too high, and you risk discomfort or circulation problems. Knowing which mmHg range suits each trimester and symptom level is key to staying comfortable and healthy as your body changes.
Compression Levels Explained
Light Compression (15–20 mmHg)
Light compression provides a gentle squeeze, perfect for early pregnancy or mild swelling. It applies minimal graduated pressure—strongest at the ankle and easing toward the calf—to support natural blood flow without feeling restrictive. Many expectant mothers start with this level to manage slight puffiness after long hours of standing or walking. It also works well for everyday wear under dresses or pants, offering subtle relief while adapting to your changing shape.
Moderate Compression (20–30 mmHg)
Moderate compression targets more noticeable swelling and early varicose veins. At 20–30 mmHg, the graduated pressure is firm enough to prevent fluid from pooling but still comfortable for daily use. This level is often recommended mid-pregnancy, when blood volume peaks and uterine weight places extra strain on leg veins. Moderate compression can reduce ankle circumference by up to one centimeter after a few hours of wear, helping you feel lighter and more energized.
Firm Compression (30–40 mmHg)
Firm compression offers the highest over-the-counter support and typically requires a doctor’s recommendation. At 30–40 mmHg, graduated pressure fights significant edema and advanced varicose veins. This level is less common in pregnancy unless you’ve developed pronounced vein issues or have a history of deep vein thrombosis. Because it’s tighter, firm compression may feel restrictive if not fitted precisely. Always consult a healthcare professional before selecting this grade.
Measuring for Accurate Fit
When to Measure
Take your measurements in the morning, before you’ve spent much time on your feet. Legs naturally swell as the day progresses, so morning readings give the truest baseline. If you measure after prolonged standing, you risk choosing a size that feels too tight later or sags when swelling increases.
How to Measure
Use a soft tape measure for three key points: the narrowest part of the ankle (just above the malleolus), the widest section of the calf, and—if you’re selecting thigh-highs—the fullest part of the thigh. Record each measurement to the nearest half centimeter. Note leg length from heel to just below the knee or to the top of the thigh, depending on the style you choose.
Importance of Fit
A precise fit ensures graduated pressure works correctly. Too loose, and blood pools below the compression zone; too tight, and circulation can be impaired. Properly fitting socks feel snug but never painful. They should stay in place all day without rolling or bunching. Accurate measurements minimize returns and guarantee you reap full benefits.
Benefits of Each mmHg Range
Benefits of 15–20 mmHg
This light grade gently eases mild ankle and foot swelling. It supports lymphatic drainage, which reduces everyday puffiness and prevents minor vein distension. Users report feeling less heaviness in their calves after just a few hours of wear, making this range ideal for first-time mothers or those with minimal discomfort.
Benefits of 20–30 mmHg
Moderate compression delivers firmer support that tackles more pronounced swelling and early varicose veins. It improves venous return by up to 30%, helping prevent blood clots and easing leg fatigue. Many pregnant women find they can stand or walk longer with less soreness, making this level a popular mid-pregnancy choice.
Benefits of 30–40 mmHg
Though less common in pregnancy, firm compression can manage severe edema and established varicosities. It provides up to 40% greater pressure at the ankle, tapering upward to maintain healthy flow. When prescribed by a physician, 30–40 mmHg socks can be a key part of a treatment plan for high-risk vein conditions.
Matching Range to Trimester
Early pregnancy often calls for 15–20 mmHg to ease minor swelling. As you move into the second and third trimesters, bump up to 20–30 mmHg to counter increased vascular strain. Reserve 30–40 mmHg for cases where a healthcare provider identifies serious venous issues. Adjusting your compression grade in step with your symptoms ensures comfort and effectiveness throughout pregnancy.
Types of Compression Materials
Nylon and Spandex Blends
Nylon and spandex dominate compression wear because they combine strength with stretch. Nylon provides durability and abrasion resistance so the sock withstands repeated use and washing. Spandex (also called elastane) delivers the elasticity needed to achieve precise mmHg ratings. Together, they produce a fabric that resists sagging while applying consistent graduated pressure. Look for blends with at least 15–20% spandex; any less and you risk rapid loss of compression after a few wears.
Microfiber Fabrics
Microfiber materials use ultra-fine synthetic fibers woven into a tight knit. Those tiny yarns create smooth, lightweight socks that feel soft against the skin. Because the fibers are so thin, there’s room for microscopically small channels that enhance breathability. Microfiber draws perspiration away from your skin without sacrificing support, making it ideal for daily wear and warmer climates. In mmHg-rated socks, microfiber helps maintain form and compression even when moisture is present.
Specialized Yarns and Coatings
Beyond basic blends, some manufacturers add functional yarns or surface treatments to boost performance. Copper-infused or silver-treated threads offer mild antimicrobial properties that reduce odor after long hours on your feet. Anti-bacterial finishes also help prevent skin irritation when you wear 20–30 mmHg daily. Other coatings can increase moisture-wicking speed or add UV protection for outdoor use. When comparing suppliers, ask for fabric performance data—percent moisture transfer, antimicrobial efficacy, and wash-to-wear retention—to ensure your chosen sock meets B2B quality standards.
Styles and Designs for Pregnancy Socks
Knee-High Versus Thigh-High
Knee-high compression is the most common format for expectant mothers. It covers from ankle to just below the knee, focusing graduated pressure where it’s needed most. Thigh-high styles extend the compression zone up to mid-thigh, offering greater support for women prone to swelling above the calf. Thigh-highs require an elastic band or silicone grip to stay in place and need very precise thigh measurements to avoid slipping or cutting in.
Open-Toe Versus Closed-Toe

Closed-toe socks provide full coverage, protecting toes and distributing pressure evenly from foot to calf. They suit cooler climates and offer more consistent graduated compression. Open-toe designs stop just before the toes, leaving them free for breathability or fitting into open-toe footwear. Many pregnant women choose open-toe in summer or when tight shoes make closed toes uncomfortable. From a manufacturing standpoint, open-toe socks are simpler to size, since you only need calf and ankle data.
Integrated Maternity Tights
For end-to-end support, some brands offer maternity tights that combine a supportive belly panel with graduated compression legs. The upper portion lifts and stabilizes the abdomen, while the leg section delivers your chosen mmHg level. Seamless construction and soft waistband designs prevent pressure points around the bump. These all-in-one solutions appeal to retailers seeking a premium, full-coverage product.
Care and Maintenance
How to Put On Compression Garments
Putting on compression socks correctly preserves their elasticity and ensures even pressure. Start by turning the sock inside out down to the heel. Slip your foot in, align the toe seam, and gently pull the fabric up to your ankle. Then, gradually unroll or pull the rest of the sock over your calf, smoothing out wrinkles as you go. If you have trouble bending, use a donning aid or gloves made for compression wear to protect the fibers.
Washing and Maintenance Tips
To protect elastic fibers, wash compression garments on a gentle cycle with cold water and a mild, pH-neutral detergent. Avoid bleach and fabric softeners, as they break down the compression yarn. After washing, reshape each sock or stocking and lay it flat to air dry—never tumble dry or expose to direct heat. Store socks rolled loosely or flat; hanging from clips can stretch the top band over time.
When to Replace Your Compression Items
Even the best compression socks wear out. Aim to replace them every three to six months, depending on how often you wear and wash them. Signs it’s time for new socks include sagging fabric, loose threads, or decreased snugness around the ankle and calf. Worn-out socks fail to maintain proper graduated pressure, reducing their ability to manage swelling and support circulation effectively.
Compression Levels Explained
Understanding mmHg Ratings
Compression socks are labeled by the amount of pressure they apply, measured in millimeters of mercury (mmHg). For pregnancy, common ranges include 15–20 mmHg, 20–30 mmHg, and 30–40 mmHg. The higher the number, the firmer the pressure. Lower levels (like 15–20 mmHg) offer light compression, often used for mild swelling or preventive care. Mid-range (20–30 mmHg) helps manage moderate swelling and discomfort. Higher ratings (30–40 mmHg) are generally reserved for those with medical needs under a healthcare provider’s direction. Understanding these numbers helps you make a choice that meets your needs without over-restricting circulation.
Which Compression Level Is Best During Pregnancy?
Most expectant mothers find 15–20 mmHg compression socks ideal. This range supports circulation and reduces swelling without feeling restrictive. It’s often recommended for daily use, especially in the second and third trimesters when swelling becomes more noticeable. If you’re experiencing varicose veins, heaviness, or prolonged standing, your doctor may suggest 20–30 mmHg compression for greater support. Avoid jumping to higher ratings without medical advice, as too much pressure can lead to discomfort or restrict blood flow. The key is consistent, gentle pressure that improves comfort while maintaining circulation.
Safety and Medical Guidance
When to Consult Your Doctor
Before using compression socks during pregnancy, especially higher compression levels, check with your OB-GYN or healthcare provider. They’ll consider your symptoms, any existing conditions like high blood pressure or blood clot risk, and recommend the appropriate level of compression. For women with preeclampsia, gestational hypertension, or a history of thrombosis, professional guidance is essential.
Signs Your Socks Are Too Tight
Compression socks should feel snug but never painful. If you experience numbness, tingling, or skin discoloration, they may be too tight or the wrong size. Red marks that don’t fade or socks that roll down suggest poor fit or incorrect application. These issues can hinder circulation instead of helping it. It’s crucial to recheck your sizing or switch to a lower compression level. A well-fitting sock will offer support, not discomfort.
Common Pregnancy Symptoms Helped by Compression Socks
Leg Swelling and Edema
One of the most frequent complaints in pregnancy is swelling, especially in the feet and ankles. Compression socks improve venous return—the upward flow of blood to the heart—helping prevent fluid buildup. Graduated compression keeps blood moving from the lower legs, where it tends to pool. Wearing socks daily can reduce the “heavy leg” feeling and improve comfort throughout the day, especially if you sit or stand for long periods.
Varicose Veins and Spider Veins
Hormonal changes and added pressure on your veins during pregnancy can cause visible veins to surface. Compression socks gently squeeze the leg tissues, supporting vein walls and reducing blood pooling. This prevents new veins from appearing and minimizes discomfort from existing ones. They don’t remove varicose veins, but they can keep symptoms from worsening and reduce aching or throbbing sensations.
Fatigue and Circulation Issues
Poor circulation during pregnancy may leave your legs feeling tired or restless. Compression socks stimulate blood flow and improve oxygen delivery to muscles, reducing that drained sensation. You’ll feel more energized with better circulation, especially during long days on your feet or travel. Improved blood flow also reduces the risk of blood clots, making these socks a preventive tool as well as a comfort aid.
Lifestyle Tips to Enhance Compression Benefits
Elevating Your Legs
After a day on your feet, simple elevation eases fluid buildup. Lie on your back and prop your lower legs on two or three pillows so your heels sit above hip level. Hold this position for 15–20 minutes, two to three times daily. Gravity assists your compression socks by encouraging pooled fluid to flow back toward your torso. Over time, you’ll notice less ankle puffiness and lighter calves, especially on warmer days or after long periods of standing.
Staying Active Safely

Gentle movement complements graduated compression. Aim for 20–30 minutes of low-impact exercise—brisk walking, swimming, or prenatal yoga—most days of the week. These activities stimulate blood flow without overtaxing your joints or muscles. Compression socks enhance each step by supporting calf muscles, reducing soreness and fatigue. Always wear well-fitting shoes and listen to your body: rest if you feel dizzy or overly tired.
Hydration and Diet
Proper fluid balance helps your compression garments work more effectively. Drink at least eight glasses of water daily to assist lymphatic drainage and prevent dehydration, which can worsen swelling. Limit salty snacks and processed foods high in sodium, as excess salt causes your body to retain water. Instead, include potassium-rich foods—bananas, avocados, sweet potatoes—to balance electrolytes. A well-rounded diet paired with compression support delivers better circulation and more consistent comfort.
Shopping and Customization Options
Off-the-Shelf vs. Custom Solutions
Standard 15–20 and 20–30 mmHg socks come in fixed sizes and are readily available online or in pharmacies. They work well for many expectant mothers, but if your measurements fall between sizes, you may experience slipping or pinching. Custom compression socks, made to your exact ankle, calf, and leg-length measurements, guarantee a precise fit. Though minimum orders start around 500 pairs and lead times extend to 3–4 weeks, custom options eliminate fit issues and allow you to choose specific fabrics or colours that reflect your brand or clinic.
Working with Manufacturers
When you opt for custom orders, share clear measurement charts and specify the mmHg range you need. Request material swatches—microfiber, moisture-wicking blends, or copper-infused yarns—to test feel and performance. Ask for a prototype before bulk production to confirm fit and compression feel. Clear communication about package design, labelling, and packaging will streamline the process and ensure you receive exactly what you expect.
Budget and Warranty Considerations
Evaluate total cost, including shipping, duties, and potential returns on standard sizes. Custom orders spread fixed costs over larger volumes, lowering per-unit prices but requiring upfront investment. Look for suppliers offering elastic-integrity warranties—guarantees that socks will maintain their mmHg rating for a specified period or number of washes. This coverage protects your clients and reinforces your reputation for quality.
Conclusion
Choosing the right mmHg range—typically 15–20 mmHg for mild swelling and 20–30 mmHg for moderate symptoms—ensures you get effective, comfortable support. Precise measurements and breathable, moisture-wicking fabrics maximize benefits. Simple habits like leg elevation, low-impact exercise, and proper hydration further enhance compression performance. With the correct compression level and fit, you can ease pregnancy-related discomfort and safeguard circulation. Whether you choose off-the-shelf or custom solutions, prioritizing quality materials and accurate sizing makes all the difference. Consult your healthcare provider for personalised advice, then partner with trusted manufacturers to deliver the best compression socks for every expectant mother.
FAQ
What mmHg level should I choose in early pregnancy?
Start with 15–20 mmHg for mild swelling and daily comfort.
Can I sleep in compression socks?
It’s best to wear them during waking hours; consult your doctor before overnight use.
How long should I wear compression socks each day?
Aim for 8–10 hours daily, removing them before bed to allow skin to breathe.
How often do I need to wash and replace them?
Wash every 2–3 wears on a gentle cycle; replace every 3–6 months or when elasticity fades.
Are there any risks to wearing higher mmHg levels?
Using 30–40 mmHg without medical advice can restrict circulation; always consult your healthcare provider first.
