Introduction: The Nighttime Compression Question
The question of whether compression socks can or should be worn to bed represents one of the most common inquiries in compression therapy. While these specialized garments have long been established as beneficial during daytime activities, their role during sleep remains less clearly defined and often surrounded by conflicting advice. This comprehensive guide explores the nuanced considerations of nighttime compression, examining the potential benefits, risks, and appropriate applications of wearing compression socks to bed. By understanding the physiological effects of overnight compression, the specific conditions that might benefit, and the important safety considerations, readers can make informed decisions about incorporating this practice into their health routines rather than relying on generalized recommendations that fail to account for individual circumstances and needs.
The Science of Overnight Compression
How Compression Affects the Body During Recumbent Positions
The physiological effects of compression therapy change significantly when transitioning from upright to recumbent positions. While standing or sitting, graduated compression works against gravity to enhance venous return and reduce fluid accumulation in the lower extremities. During recumbent sleep, however, the gravitational challenges diminish as the legs elevate to approximately the same level as the heart, naturally improving circulation without external assistance. This positional change alters the fundamental dynamics of compression therapy, potentially reducing its necessity for some individuals while remaining beneficial for others with specific circulatory challenges. Understanding these position-dependent effects helps explain why nighttime compression recommendations differ from daytime guidelines and why personalized approaches become particularly important when considering overnight use.
Circulation Changes During Sleep Cycles
Sleep introduces complex circulatory patterns that interact with compression therapy in ways distinct from waking hours. During normal sleep cycles, the body experiences natural fluctuations in blood pressure, heart rate, and peripheral circulation as it moves through different sleep stages. These natural variations can both complement and occasionally conflict with the effects of sustained compression. For some individuals, the consistent external pressure from compression socks helps stabilize circulatory patterns throughout sleep cycles, while for others, it might interfere with the body’s natural nocturnal circulatory regulation. These interactions between sleep physiology and compression effects explain why some people experience improved sleep quality with nighttime compression while others report discomfort or disrupted sleep, highlighting the importance of individual assessment rather than universal recommendations.
| Position | Compression Effect | Circulatory Impact | Clinical Relevance |
|---|---|---|---|
| Upright (Standing/Sitting) | Enhances venous return against gravity | Reduces swelling, prevents pooling | Standard use for varicose veins, DVT, fatigue |
| Recumbent (Lying Down) | Less needed due to horizontal position | Natural circulation improves with elevation | Used only when medical conditions require |
| During Sleep Cycles | May stabilize or disrupt blood flow patterns | Circulation fluctuates with sleep stages | Should be prescribed based on individual needs |
Medical Perspectives on Nighttime Compression
Conditions That May Benefit from Overnight Compression
Several specific medical conditions present circumstances where the benefits of nighttime compression may outweigh potential drawbacks. Patients with severe venous insufficiency often experience nocturnal symptoms like cramping and restless legs that can significantly disrupt sleep quality, with overnight compression potentially providing symptomatic relief. Those with post-thrombotic syndrome following deep vein thrombosis may benefit from continuous compression to manage persistent swelling and discomfort. Lymphedema patients frequently require round-the-clock compression to maintain fluid balance, particularly during early treatment phases. Individuals recovering from certain surgical procedures or injuries might receive specific instructions for overnight compression to support healing processes. These condition-specific applications highlight situations where medical providers might recommend nighttime compression as part of a comprehensive treatment approach, typically with specific guidance on appropriate compression levels and monitoring protocols.
When Nighttime Compression Should Be Avoided
Despite potential benefits for some conditions, several circumstances present clear contraindications for overnight compression use. Patients with peripheral arterial disease or significant arterial insufficiency should generally avoid nighttime compression due to risks of further restricting already compromised blood flow during periods of reduced movement. Those with certain skin conditions, particularly those affecting skin integrity or sensation, may face increased risks of tissue damage from prolonged compression without regular position changes and skin checks. Individuals with cardiac conditions causing fluid balance challenges require careful assessment, as nighttime compression can potentially affect cardiac preload and fluid distribution patterns. These contraindications emphasize the importance of professional medical evaluation before initiating overnight compression, particularly for individuals with complex health histories or multiple chronic conditions that might create competing risk-benefit considerations.
Compression Garment Selection for Night Use
Choosing the correct type of compression garment for nighttime wear is critical for comfort and safety. Low to moderate compression levels (typically 15–20 mmHg) are often preferred for overnight use, as they reduce the risk of circulatory restriction while still offering therapeutic benefits. Seamless designs and soft, breathable fabrics help prevent skin irritation during extended wear. Some products are specifically labeled as “nighttime compression” and incorporate features like extra cushioning or graduated tension zones. Consulting with a medical professional ensures the selected sock aligns with individual health needs and avoids unintended complications from prolonged nighttime use.
Comfort and Sleep Quality Considerations
The relationship between compression garments and sleep quality varies significantly among individuals, with both potential benefits and challenges to consider. For some users, the consistent pressure sensation creates a calming proprioceptive input that facilitates faster sleep onset and fewer nighttime awakenings, particularly for those with restless leg symptoms or nocturnal cramping. Conversely, others experience the constant pressure as an irritating sensation that interferes with natural sleep initiation or causes disruptive awareness during lighter sleep phases. The garment’s physical presence may also create mechanical sleep disruptions through movement restriction or bunching during position changes. These varied experiences highlight why personal experimentation under appropriate medical guidance often proves necessary to determine individual sleep compatibility with compression garments, with attention to both subjective sleep quality measures and objective indicators like morning symptoms and overall restfulness.
Temperature management represents a significant consideration for overnight compression use, as sleep quality depends heavily on appropriate thermoregulation. Compression garments create an additional layer that can potentially interfere with the body’s natural cooling mechanisms during sleep, particularly in warm environments or for individuals who naturally experience elevated body temperatures during rest. This thermal effect can disrupt the normal body temperature decrease that facilitates quality sleep, potentially leading to increased wakefulness or reduced deep sleep phases. Conversely, in cooler environments, the additional layer might enhance comfort for those who experience cold extremities during sleep. Material selection becomes particularly important for overnight use, with moisture-wicking fabrics and temperature-regulating technologies offering potential solutions to these thermoregulation challenges while maintaining therapeutic compression benefits.
Selecting Appropriate Nighttime Compression
Compression Levels for Overnight Use
The appropriate compression level for nighttime use typically differs from daytime recommendations, requiring careful consideration of both therapeutic needs and safety factors. While daytime compression often ranges from 15-30+ mmHg depending on the condition being addressed, nighttime compression generally trends toward the lower end of this spectrum to balance therapeutic benefits with comfort and safety during periods of reduced movement and monitoring. Mild compression (8-15 mmHg) often provides sufficient benefit for preventive purposes or minor symptoms while minimizing risks during sleep. Moderate compression (15-20 mmHg) may be appropriate for specific conditions under medical guidance, while higher levels typically require explicit medical direction with clear monitoring protocols. This conservative approach to nighttime compression levels reflects the reduced need for gravitational assistance during recumbent positions and the increased importance of comfort for sleep quality maintenance.
Material and Design Features for Comfort
Material selection and design elements take on heightened importance for compression garments intended for overnight use, with several specific features contributing to both comfort and safety. Seamless construction minimizes pressure points that might become problematic during extended wear periods, while soft, non-abrasive fabrics reduce skin irritation risks during the natural movement that occurs during sleep cycles. Moisture-wicking properties help manage the perspiration that can accumulate under compression garments, preventing skin maceration that increases tissue vulnerability. Non-constrictive top bands prevent uncomfortable constriction while maintaining proper garment positioning throughout the night. Some specialized nighttime compression options incorporate graduated designs with slightly reduced pressure in areas prone to nerve compression during recumbent positions. These thoughtful design elements can significantly impact both the comfort and safety profile of compression garments intended for overnight use.
Professional Recommendations and Guidelines
What Medical Providers Advise

Medical guidance regarding overnight compression varies based on specialty, patient population, and individual practitioner experience, though several consistent themes emerge across professional recommendations. Vascular specialists typically emphasize individualized assessment rather than blanket recommendations, considering each patient’s specific circulatory status, symptoms, and risk factors when advising about nighttime compression. Wound care specialists often support overnight compression for patients with venous ulcers or significant edema affecting wound healing, while emphasizing proper fit and regular skin monitoring. Lymphedema therapists frequently incorporate nighttime compression into treatment protocols, particularly during intensive therapy phases, though often with specialized garments designed specifically for overnight use. These nuanced professional perspectives highlight why patients should seek personalized medical advice rather than following general guidelines, particularly when considering compression use for specific medical conditions rather than general wellness purposes.
Evidence-Based Approaches to Overnight Use
The research evidence regarding overnight compression presents a complex picture that continues evolving as more studies examine specific applications and outcomes. Clinical trials investigating continuous compression for severe venous insufficiency have demonstrated symptom improvements for selected patients, particularly those with nocturnal cramping or significant evening edema. Studies examining lymphedema management consistently support round-the-clock compression during intensive treatment phases, though with careful monitoring protocols. Research on post-thrombotic syndrome suggests potential benefits from extended compression wear times, including overnight use, for symptom management in selected patients. However, studies also document increased risks of skin complications with prolonged uninterrupted compression, particularly in populations with compromised sensation or circulation. This mixed evidence base reinforces the importance of individualized approaches guided by healthcare providers familiar with both the potential benefits and risks based on current research rather than generalized recommendations.
Practical Implementation Strategies
Establishing a Safe Nighttime Routine
Implementing overnight compression safely requires establishing structured routines that balance potential benefits with appropriate monitoring and risk management. A comprehensive approach includes thorough evening skin inspection before application, ensuring the absence of concerning changes like unusual redness, breaks in skin integrity, or new discomfort. Proper application technique becomes particularly important, avoiding wrinkles or uneven pressure distribution that could create problems during extended wear. Some practitioners recommend brief removal periods before sleep to allow skin assessment and short breaks from compression. Morning routines should include prompt removal upon waking, followed by thorough skin inspection and appropriate hygiene measures. For individuals with reduced sensation or mobility limitations, caregiver assistance with these routines may be necessary to ensure safety. These structured approaches help minimize risks while maximizing potential benefits from overnight compression when medically appropriate.
Monitoring for Complications
Vigilant monitoring for potential complications represents an essential component of safe overnight compression use, with several specific warning signs warranting immediate attention. Users should establish baseline awareness of normal skin appearance and sensation to recognize concerning changes quickly. Morning skin inspection should focus on identifying persistent indentations, unusual discoloration (particularly whiteness or purple/blue tones), increased pain or numbness, and any signs of skin breakdown. Symptoms like increased pain during the night, new numbness or tingling, or color changes visible through the garment warrant immediate removal and assessment. Some providers recommend periodic overnight breaks from compression to evaluate how symptoms respond to intermittent rather than continuous use. This monitoring approach acknowledges that the risk-benefit balance of overnight compression requires ongoing assessment rather than one-time determination, with adjustments based on observed responses and changing health conditions.
Selecting Appropriate Compression Levels
Choosing the correct compression level is critical for safe overnight use. Most healthcare professionals recommend mild to moderate pressure (8–20 mmHg) for sleep. Higher levels may increase risk during prolonged wear unless under medical supervision. When in doubt, start with lower compression and monitor body response before progressing. Socks should fit snugly but not feel tight or cause discomfort. Always consult a medical professional for guidance if there are pre-existing circulatory issues, diabetes, or skin sensitivity. Proper selection ensures effectiveness while minimizing complications associated with improper compression levels during rest.
| Special Population / Scenario | Key Considerations | Recommended Compression Level | Additional Notes |
|---|---|---|---|
| Pregnancy (Third Trimester) | Increased venous pressure and swelling | Mild to moderate (10-20 mmHg) | Medical consultation advised; specialized maternity compression recommended |
| Postpartum (Including C-Section) | Persistent edema, thrombosis risk | Mild to moderate (10-20 mmHg) | Close medical monitoring needed; garments designed for postpartum use preferred |
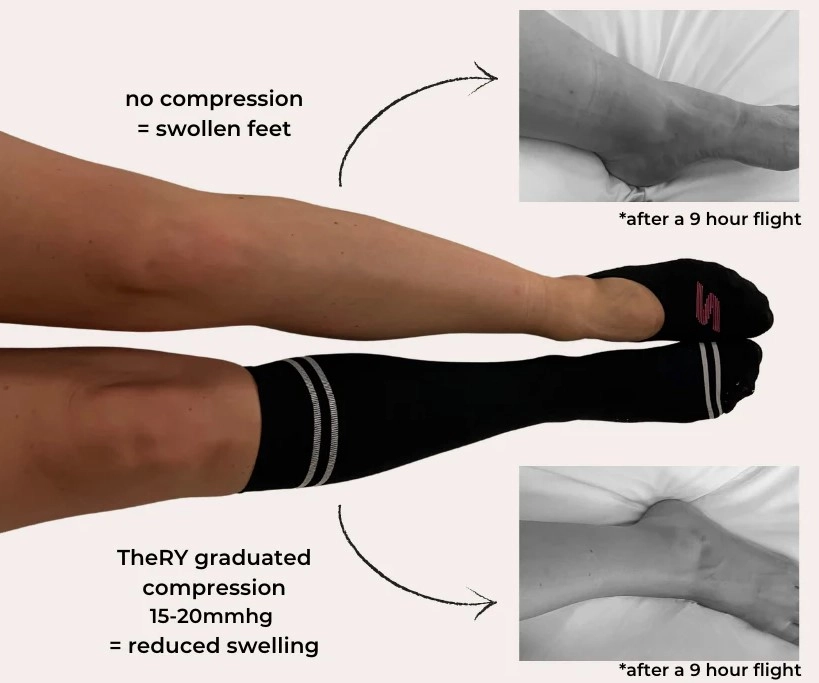
| Long-Distance Travel & Overnight Flights | Prolonged immobility, low cabin pressure, thrombosis risk | Moderate (15-20 mmHg) | Combine with regular movement, hydration; avoid sedatives |
| General Overnight Use | Cautious approach due to possible circulation changes | Individualized | Medical guidance strongly recommended |
Special Populations and Considerations
Pregnancy and Postpartum Applications
Pregnancy and the postpartum period present unique considerations for overnight compression use, with both potential benefits and specific cautions. During pregnancy, the significant circulatory changes and increased venous pressure often lead to substantial lower extremity swelling and discomfort that may persist into nighttime hours. For some expectant mothers, particularly in the third trimester, mild to moderate overnight compression may help manage these symptoms and improve sleep quality. The postpartum period brings different considerations, with some women experiencing persistent edema or increased thrombosis risk, particularly following cesarean delivery. In both circumstances, medical guidance becomes especially important, as the normal physiological changes of pregnancy and postpartum recovery interact with compression effects in complex ways. Specialized maternity compression garments designed for the unique needs of pregnant and postpartum women may offer better comfort and appropriate pressure distribution compared to standard options.
Travel Considerations and Overnight Flights
Long-distance travel, particularly overnight flights, presents specific circumstances where nighttime compression garments may offer significant benefits despite general cautions about overnight use. The combination of prolonged sitting, reduced mobility, lower cabin pressure, and disrupted sleep creates ideal conditions for fluid accumulation and increased thrombosis risk during air travel. In these specific circumstances, many medical providers actively recommend compression garments throughout the journey, including sleep periods, particularly for individuals with additional risk factors for blood clots. The compression levels typically recommended for travel (15-20 mmHg) balance thrombosis prevention with comfort during extended wear. Travelers should implement additional protective measures alongside compression, including regular movement when possible, proper hydration, and avoiding sleep medications that might further reduce movement during flight. These travel-specific recommendations highlight how context significantly influences the risk-benefit assessment for overnight compression use.
Alternative Approaches to Nighttime Leg Health
Elevation Strategies and Techniques
For individuals seeking alternatives to overnight compression or complementary approaches to enhance its benefits, strategic elevation offers significant advantages for nocturnal leg health. Properly positioned elevation places the legs above heart level, utilizing gravity to naturally enhance venous return and fluid drainage without the potential drawbacks of continuous compression. Effective elevation typically requires raising the legs 6-12 inches using specialized pillows, foam wedges, or adjustable bed features rather than simply stacking standard pillows that might create awkward angles or pressure points. The optimal elevation angle balances circulatory benefits with sleep comfort, typically around 15-20 degrees for most individuals. This approach proves particularly valuable for those with mild to moderate symptoms or contraindications to overnight compression, though individuals with severe conditions may benefit from combining appropriate elevation with medical-grade compression under healthcare supervision.
Evening Routines to Minimize Overnight Swelling
Proactive evening routines can significantly reduce nocturnal swelling and discomfort without necessarily requiring overnight compression garments. Implementing a structured wind-down period that includes 15-20 minutes of gentle elevation before sleep helps initiate the fluid redistribution process before entering sleep cycles. Brief self-massage using effleurage techniques (light, flowing strokes moving toward the heart) can enhance fluid movement from extremities. Avoiding excessive salt consumption in evening meals helps minimize overnight fluid retention, while proper hydration throughout the day—rather than catching up with large fluid volumes before bed—supports overall circulatory health. Some individuals benefit from gentle ankle pumping exercises before sleep to activate the calf muscle pump mechanism. These complementary approaches can either replace overnight compression for those with mild symptoms or enhance its effectiveness for those with medical indications for nighttime compression use.
Conclusion: Making an Informed Decision About Nighttime Compression
The question of whether compression socks should be worn to bed does not have a universal answer applicable to all individuals. Instead, this decision requires thoughtful consideration of personal health circumstances, specific symptoms, risk factors, and quality of life impacts. For some individuals—particularly those with severe venous insufficiency, lymphedema, or post-thrombotic syndrome—the benefits of overnight compression may outweigh potential risks when implemented with appropriate medical guidance and monitoring protocols. For others, the risks may exceed potential benefits, making alternative approaches to nighttime leg health more appropriate.

This nuanced perspective emphasizes the importance of individualized assessment rather than generalized recommendations. By understanding the physiological principles, potential benefits, risks, and alternatives outlined in this guide, readers can engage in more informed discussions with healthcare providers about whether overnight compression might be appropriate for their specific circumstances. This collaborative approach to decision-making, combining medical expertise with personal preferences and practical considerations, offers the best path to optimizing both leg health and sleep quality—whether that ultimately includes overnight compression or alternative management strategies tailored to individual needs.
If you’re interested in high-quality, customized compression socks designed to meet specific needs, we invite you to explore our website. At Max Hosiery, we provide tailored solutions that combine comfort, durability, and performance. Contact us today to discuss how we can help you or your business customize socks that deliver both function and style.
FAQ Section
Is it dangerous to wear compression socks to bed every night?
While not universally dangerous, nightly use requires appropriate medical guidance, as risks vary based on individual health conditions; those with arterial insufficiency, neuropathy, or skin integrity issues face higher risks, while others with specific conditions like severe venous insufficiency may benefit from properly supervised overnight use.
What compression strength is best for overnight wear?
Lower compression levels (8-15 mmHg) are generally safer for overnight use when appropriate, as they provide therapeutic benefit with reduced risk during periods of limited movement and monitoring; higher levels should only be used overnight with specific medical direction and clear monitoring protocols.
Can wearing compression socks at night worsen circulation for some people?
Yes, particularly for those with arterial insufficiency or peripheral artery disease, as the external pressure could further restrict already compromised arterial blood flow during periods of reduced movement; this highlights why medical assessment before initiating overnight compression is essential.
How do I know if overnight compression is helping or hurting me?
Monitor morning symptoms (reduced vs. increased swelling/pain), sleep quality, skin condition after removal, and any new discomfort or numbness; improvement in symptoms without new issues suggests benefit, while new pain, numbness, skin changes, or worsened symptoms indicate potential problems requiring medical consultation.
Are there special compression socks designed specifically for sleep?
Yes, specialized nighttime compression garments feature softer materials, reduced pressure in areas vulnerable during recumbent positions, non-constrictive bands, and seamless construction for extended comfort; these purpose-designed options may offer better safety profiles than wearing standard daytime compression garments to bed.
